LAPAROSCOPIC INCONTINENCE SURGERY

Director of the Sydney Women’s Endosurgery Centre ( SWEC), Australia’s leading Centre for the development and training in Advanced Laparoscopic Surgery for Women and Director of the St George Urodynamic Centre for Pelvic Floor Disorders
WHAT IS SRESS INCONTINENCE?
This is the leakage of urine during times of exertion. It usually causes the symptoms of stress, cough or sneeze induced leakage. There is a lifetime risk of 25-50% of women complaining of urinary stress incontinence. When this results in a significant effect on lifestyle, patients may seek treatment that may include surgery.
HOW CAN IT BE TREATED?
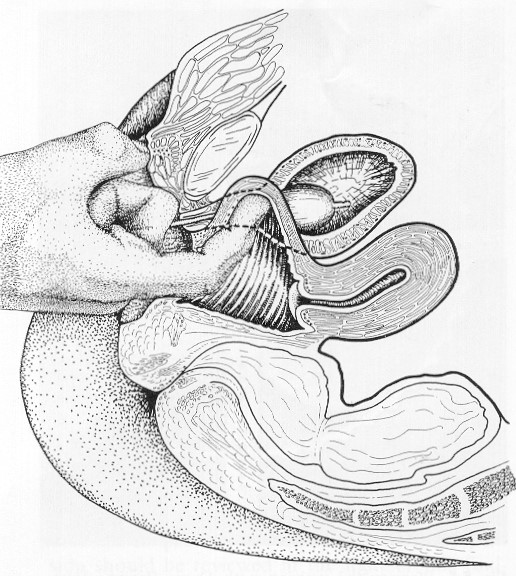
When conservative measures such as Pelvic Floor Physiotherapy, intravaginal appliances (ring pessaries), lifestyle changes and weight loss have failed patients will usually present for a surgical option. The Gold Standard for the treatment of Genuine Stress Incontinence due to weakness of the bladder neck has historically been the Burch Colposuspension since it was first reported in l961. There are numerous long term studies of up to 10 years following surgery that support this. This bladder neck weakness is caused by childbirth, congenital factors and the tissue softening associated with the menopause. We have performed over 1000 of these procedures with a success rate of around 90% using the open technique with a transverse caesarean” type scar. The operation involves the stitching of the bladder neck to the ligaments at the back of the pubic bone. This prevents the bladder valve from dropping during a cough, which would cause it to open up and lose urine. This 10-15 cm “bikini cut” incision meant a considerable amount of postoperative pain requiring heavy narcotic analgesia, prolonged postoperative catheter drainage, and worst of all, a 5-7 day hospital stay and 4-6 weeks off work. This meant that many women had to persevere with their symptoms rather than commit to this major abdominal surgery and prolonged convalescence.
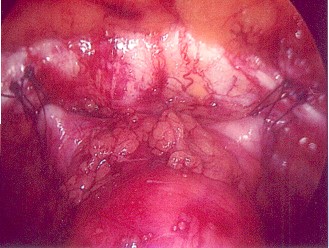
In 1991 we were the first to perform this operation in Australia using the new techniques of advanced laparoscopic or keyhole surgery and since then we have been performing this procedure with exactly the same results (ANZJOG 1996 36:1:44) In 2003 we reported the long term results of over 500 cases, 5-10 years after surgery with a subjective success rate of 85%. Laparoscopy allows us to better visualise all the anatomy, the various areas of weakness and repair these site specific defects in a more anatomical way, often repairing multiple defects at the same surgery. In 2012 we began using Robotic surgery to perform many of these operations.
We also found that because there were no large incisions there was very little postoperative pain and therefore little need for postoperative catheter drainage with a bag to establish early normal voiding. The average patient went home on the 2nd postoperative day without a catheter and was back to normal activities around the house and work in 1-2 weeks respectively. Fifteen percent of patients required catheterisation for longer than 48 hours after an unsuccessful trial of void. Most of these still went home very early on day 2-3 with the very modern forms of simple continuous bladder drainage using an indwelling urethral catheter and a leg bag or a simple suprapubic catheter. Patients then return to the ward again on day 5-7 for a repeat trial of void which is successful in over 80% of cases.
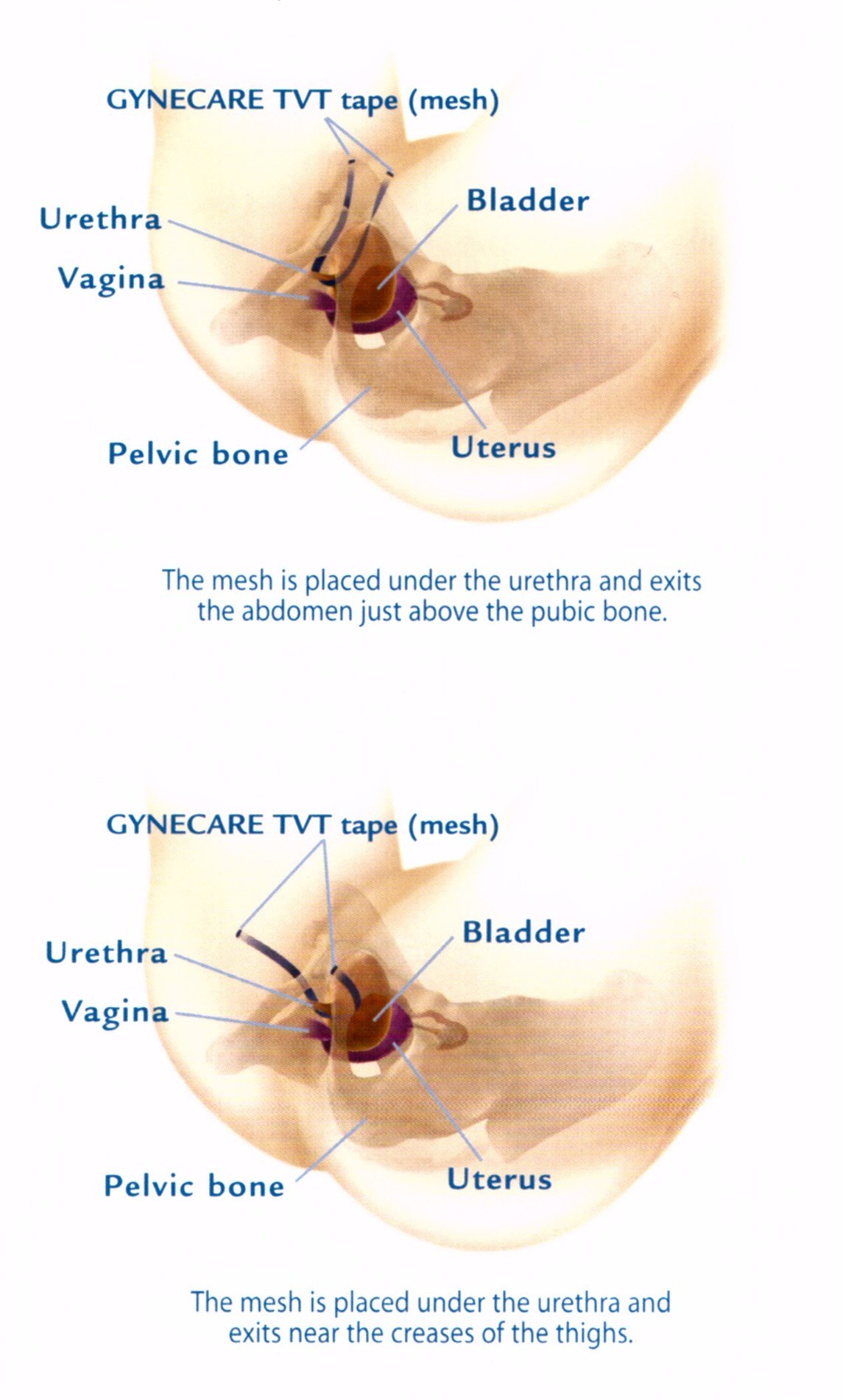
TVT Suburethral Tapes
In 1996 the TVT tape was released onto the market to treat simple stress incontinence without prolapse. This was launched as an alternative to the Laparoscopic Burch Colposuspension for patients without prolapse and for patients who were a poor risk for laparoscopic surgery such as the elderly or those with major medical conditions which might require a longer general anaesthetic. This technique uses a small mesh strip placed around the midportion of the urethra and pulled out either behind the pubic bone or in the groin region. This tape has a “Velcro like” which does not require stitching to kink the bladder neck with exertion and can usually require a hospitalisation of around 24 hours. Although vaginal mesh complications have received a lot of attention in the media these small tapes or slings have a very low complication rate and have been a very valuable addition to minimally invasive incontinence surgery over the last 15 years.
The major advantages of Laparoscopic Burch Colposuspension over TVT tapes is that NO MESH is required to achieve the same success rates and accompanying prolapse (particularly bladder and apical prolapse) can be fixed with the same operation without any vaginal surgery or mesh at all once again with similar success rates.
IS THE OPERATION SAFE?
Complications are similar to those of the open and vaginal operations except that the incidence of wound infection is drastically reduced. These complications include those of any general anaesthesia and major pelvic operation including haemorrhage, infection, thrombosis and inadvertent injury to the bladder, bowel or major vessels. This rate is approximately 5 cases per 1000. There is also a failure rate of 10% in the first 5 years after surgery. Overactive bladder symptoms of urgency and sometimes urge leakage can occur in 15% of cases in the 6 weeks after the surgery but usually settle completely with simple bladder drill and medication.
POSTOPERATIVE INSTRUCTIONS
For patients after Laparoscopic Incontinence or Pelvic Floor Reconstruction and TVTS
Following your operation you will return to the ward with an indwelling urethral catheter or suprapubic catheter or no catheter at all. You will also have a dressing over the 3-5 small puncture incisions at the umbilicus and on the right and left side above the hip and in the groins for TVT-O. You may also be experiencing post laparoscopy pain which is usually mild to moderate but may be enough to require an injection to settle you early on. It can be felt as a generalised abdominal pain or a colicky wind like pain with bloating and pressure under your ribs or shoulder tip pain. It usually lasts from 4-24 hours and I stress it is usually not a major problem although it can be annoying and painful. You will not need any injections after 6 am the following morning. The nursing staff will give you tablets or suppositories which give excellent pain relief without sedation from then on. You may also experience postoperative nausea within the first 12 hours and therefore you will have an IV infusion to give you fluids. This drip is usually removed the following morning and you are encouraged to eat and drink freely. .
The next day you will be mobilized very early to help accelerate your recovery and your bladder and bowel function. If there is a catheter in place it will be removed and then you will be encouraged to void. Here are some rules to help you:-
- Go to the toilet whenever you feel the normal sensation to go, but never leave it longer than 4 hours without emptying your bladder. You may need to try on a number of occasions. Following this, your residual urine will be assessed by using a simple bladder scan performed by your nurse.
- If you are going very frequently and passing small amounts only, then is it likely that you have some retention of urine. Don’t worry as the nurse will pass a small in and out catheter from time to time until your voiding well with residuals (what is left in your bladder after you void) less than 100 mls on at least two occasions.
- If you have burning or scalding or bladder pain you may have an infection. Tell the nurse or let me know as a sample must be taken and usually an antibiotic prescribed.
When passing your urine it is best to relax and not force your urine. You must remember that the operation is supposed to hitch up your bladder valve and obstruct your flow. Before your operation when your bladder was weak, you usually emptied your bladder by just dropping your pelvic floor and the urine fell out. If the operation is a success it means that when you drop your pelvic floor muscles, nothing will happen, and you will have to expel the urine using your bladder detrusor muscle. With long term weak bladders the muscle may be lazy and take some time to regain its power. It doesn’t matter and merely is a short-term nuisance.
- The bladder empties best by sitting on the toilet with your weight forward on your toes, not on your heels, even if this means lifting your bottom off the seat. This is called the “double voiding”
- If you are one of a group of about 15% who still have voiding problems then we can insert a simple indwelling urethral catheter which is left on free drainage for your discharge, or a suprapubic catheter inserted in the ward or at the time of your operation to allow you to void normally and then test your residual at home just by sliding a valve on the tubing and not by inserting anything. You will still go home early. Only 15% of patients need any form of catheter after 48 hours.
- 15% of patients develop an irritable or unstable bladder after this type of incontinence operation and this can cause unwanted bladder contractions that give you frequency, urgency and even urgency leakage with the loss of even large amounts of urine immediately after the operation. With normal operations you have a catheter for up to 5 days with a bag draining freely before you even try to pass urine so you don’t notice it so much because your bladder is empty. Because you use your bladder straight away these symptoms are more evident. Don’t worry as this is normal and doesn’t have anything to do with the success of your operation. It is usually gone within a few days but may last in a minor fashion for up to 6 weeks.
- If you have any problems after leaving hospital particularly with unusually severe pain, nausea and vomiting, hot and cold chills or fevers or voiding problems, then ring my rooms, contact Sister on her emergency mobile number that will be given to you prior to surgery or contact the nurse at the ward of your hospital for advice. If you have any problems overnight or after hours (inability voiding, incomplete voiding, severe frequency, urgency or incontinence) you can simply ring the ward at the hospital of your operation to speak to the Sister. If the catheter needs to be replaced after hours, this can be done at any time by the sister on your ward. Remember that difficulty voiding is a very common and a normal event after pelvic floor and incontinence surgery due to the nature of the stitches or mesh placed around the urethra and the dramatic change of position of the bladder. It does not matter if you void successfully on day 1, day 5, day 10 or thereafter. It does not interfere with your recovery after the operation and is a temporary inconvenience to you. It has no relationship to the final outcome of your surgery. You must relax, relax, relax and your bladder will empty properly only when it is ready. Straining will do nothing to improve your success.
- Return for your postoperative visit at 4-6 weeks as organized by my secretary.
9 The dressings on your port sites are taken off usually after one day and almost always the stitches are dissolvable, usually invisible below the skin and do not need to be removed by your Doctor.
Remember that as soon as you go home you can drive a car, carry out light household duties, and begin low impact exercise such as walking. You can’t have intercourse, lift over 20 KG or indulge in strenuous high impact exertion until you see me for your postoperative check up at 6-8weeks. This is because the suture slings that hold the bladder neck in place need to scar securely to weld the structure in place for a permanent cure. Don’t worry about coughing or sneezing by accident, as this will do no harm at all and you should be dry.
WHAT IS THE COST OF THIS PROCEDURE?
This practice charges the fees set by the AMA in most cases. The Medicare schedule does not reflect the difficulty or complexity of advanced minimally invasive surgery Advanced laparoscopic surgery requires many years to master and is only performed by a small group of surgeons in Australia who are certified to perform this operation in particular. It may take up to 2 times longer than the open operation yet only attracts the same Medicare rebate. The Medicare system considers operations like this in a similar fashion to plastic surgery where there is a very poor rebate. They feel that the great cosmetic advantage and early release from hospital as well as early return to work are a luxury that people should pay for. There is therefore a considerable gap to pay despite our attempts to lobby the government for a review.
The exact fees and gaps can be easily obtained from my secretary prior to the operation and from the anaesthetist and hospital in a similar fashion. Obviously the big decrease in hospital bed days and the early return to family and work do offset the gap considerably. Please discuss this with me if you have a problem.